Cytokinetics Announces Results From REDWOOD-HCM and GALACTIC-HF Presented in Late Breaking Clinical Trial Session at the HFSA Annual Scientific Meeting
Full Results from REDWOOD-HCM Demonstrate Improvements in Biomarkers and Heart Failure Symptoms in Patients with Obstructive Hypertrophic Cardiomyopathy Treated with Aficamten Supporting Progression to Phase 3 Clinical Trial
Additional Results from GALACTIC-HF Show Effect of Treatment with Omecamtiv Mecarbil in Black Patients Consistent with Overall Population and White Patients
REDWOOD-HCM: Full Results Demonstrate Improvements in LVOT-G, NT-proBNP and NYHA Class in Patients Treated with Aficamten with Reversibility After Discontinuation
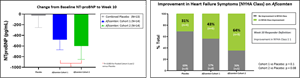
Reductions in LVOT-G occurred within two weeks of initiating treatment with aficamten, were maximized within two to six weeks of the start of dose titration and were sustained until the end of treatment at 10 weeks. Reversibility of the pharmacodynamic effect of aficamten was seen after a two-week washout, with resting LVOT-G, post-Valsalva LVOT-G, NT-proBNP and LVEF returning to baseline values. The observed reductions in LVOT-G were dose dependent, with patients achieving greater reductions of LVOT-G with increasing doses of aficamten. Over the 10-week study period, patients treated with aficamten in both Cohort 1 and Cohort 2 also experienced statistically significant reductions in NT-proBNP (p=0.003) (Figure 1). Treatment with aficamten was also associated with an improvement in heart failure functional class as measured by
Figure 1. Change from Baseline in NT-proBNP and NYHA Class is available at https://www.globenewswire.com/NewsRoom/AttachmentNg/04143a1d-b002-4ac6-b3b7-70ccbf60c25a
Treatment with aficamten in REDWOOD-HCM was generally well tolerated. Overall, the incidence of adverse events was similar between treatment arms, there were no treatment emergent adverse events that resulted in treatment interruption or discontinuation, and no serious adverse events ascribed to aficamten by investigators. All patients completed treatment per protocol.
“Results from REDWOOD-HCM underscore the potential clinical utility of aficamten based on the elimination of resting
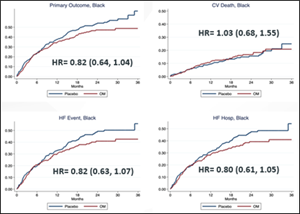
GALACTIC-HF: Outcomes in Black Patients Treated with Omecamtiv Mecarbil Similar to Overall Population and to White Patients
Figure 2. Primary Outcome in Black Patients Enrolled in GALACTIC-HF is available at https://www.globenewswire.com/NewsRoom/AttachmentNg/e62cddd3-b548-422a-8207-a0b2a52d133e
A great majority of Black patients in GALACTIC-HF (n=535, 95%) were enrolled in
“These analyses are particularly important because compared to other racial or ethnic groups Black patients have higher risk of heart failure, worse outcomes, and have historically been underrepresented in clinical research,” said
Conference Call and Webcast Information
Members of Cytokinetics’ senior management team will host a conference call and webcast tomorrow,
An archived replay of the webcast will be available via Cytokinetics’ website until
About Aficamten
Aficamten is an investigational selective, small molecule cardiac myosin inhibitor discovered following an extensive chemical optimization program that was conducted with careful attention to therapeutic index and pharmacokinetic properties that may translate into next-in-class potential in clinical development. Aficamten was designed to reduce the number of active actin-myosin cross bridges during each cardiac cycle and consequently suppress myocardial hypercontractility that is associated with hypertrophic cardiomyopathy (HCM). In preclinical models, aficamten reduced myocardial contractility by binding directly to cardiac myosin at a distinct and selective allosteric binding site, thereby preventing myosin from entering a force producing state.
The development program for aficamten is assessing its potential for the treatment of HCM and to improve exercise capacity and relieve symptoms in patients with hyperdynamic ventricular contraction and includes REDWOOD-HCM, a Phase 2 clinical trial designed to evaluate the effect of treatment with aficamten compared to placebo on measures of safety, tolerability as well as pharmacodynamics and biomarkers.
About Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is a disease in which the heart muscle (myocardium) becomes abnormally thick (hypertrophied). The thickening of cardiac muscle leads to the inside of the left ventricle becoming smaller and stiffer, and thus the ventricle becomes less able to relax and fill with blood. This ultimately limits the heart’s pumping function, resulting in symptoms including chest pain, dizziness, shortness of breath, or fainting during physical activity. A subset of patients with HCM are at high risk of progressive disease which can lead to atrial fibrillation, stroke and death due to arrhythmias. There are no FDA approved medical treatments that directly address the hypercontractility that underlies HCM.
About Omecamtiv Mecarbil
Omecamtiv mecarbil is an investigational, selective, small molecule cardiac myosin activator, the first of a novel class of myotropes1 designed to directly target the contractile mechanisms of the heart, binding to and recruiting more cardiac myosin heads to interact with actin during systole. Omecamtiv mecarbil was designed to increase the number of active actin-myosin cross bridges during each cardiac cycle and consequently augment the impaired contractility that is associated with heart failure with reduced ejection fraction (HFrEF). Preclinical research has shown that omecamtiv mecarbil increases cardiac contractility without increasing intracellular myocyte calcium concentrations or myocardial oxygen consumption.2-4
The development program for omecamtiv mecarbil is assessing its potential for the treatment of HFrEF and includes GALACTIC-HF and METEORIC-HF, a Phase 3 clinical trial designed to evaluate the effect of treatment with omecamtiv mecarbil compared to placebo on exercise capacity.
About Heart Failure
Heart failure is a grievous condition that affects more than 64 million people worldwide5 about half of whom have reduced left ventricular function.6,7 It is the leading cause of hospitalization and readmission in people age 65 and older.8,9 Despite broad use of standard treatments and advances in care, the prognosis for patients with heart failure is poor.10 An estimated one in five people over the age of 40 are at risk of developing heart failure, and approximately 50 percent of people diagnosed with heart failure will die within five years of initial hospitalization.11,12 More than 2 million people in the
About
For additional information about Cytokinetics, visit www.cytokinetics.com and follow us on Twitter, LinkedIn, Facebook and YouTube.
Forward-Looking Statements
This press release contains forward-looking statements for purposes of the Private Securities Litigation Reform Act of 1995 (the "Act").
Contact:
Senior Vice President, Corporate Communications, Investor Relations
(415) 290-7757
References:
- Psotka MA, Gottlieb SS, Francis GS et al. Cardiac Calcitropes, Myotropes, and Mitotropes. JACC. 2019; 73:2345-53.
- Planelles-Herrero VJ, Hartman JJ, Robert-Paganin J. et al. Mechanistic and structural basis for activation of cardiac myosin force production by omecamtiv mecarbil.
Nat Commun . 2017;8:190. - Shen YT, Malik FI, Zhao X, et al. Improvement of cardiac function by a cardiac myosin activator in conscious dogs with systolic heart failure. Circ Heart Fail. 2010; 3: 522-27.
- Malik FI, Hartman JJ, Elias KA, Morgan BP, Rodriguez H, Brejc K, Anderson RL, Sueoka SH, Lee KH, Finer JT, Sakowicz R. Cardiac myosin activation: a potential therapeutic approach for systolic heart failure. Science. 2011 Mar 18;331(6023):1439-43.
- James et al. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators.
Lancet 2018; 392: 1789–858. - Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:e240-e327.
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200.
- Roger VL. Epidemiology of Heart Failure.
Circulation Research . 2013;113:646-659, originally published August 29, 2013. Doi: 10.1161/CIRCRESAHA.113.300268. - Kilgore M, Patel HK, Kielhorn A et al. Economic burden of hospitalizations of Medicare beneficiaries with heart failure. Risk Manag Healthc Policy. 2017; 10: 63-70.
- Jhund PS, MacIntyre K, Simpson CR, et al. Long-Term Trends in First Hospitalization for Heart Failure and Subsequent Survival Between 1986 and 2003. Circulation. 2009;119:515-523.
- Benjamin EJ, Virani SS, Callaway CW et al. Heart Disease and Stroke Statistics—2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67-e492.
- Roger VL, Weston SA, Redfield MM, et al. Trends in Heart Failure Incidence and Survival in a Community-Based Population. JAMA. 2004;292:344-350.
- Shannon M. Dunlay, Véronique L. Roger, Susan A.
Weston , Ruoxiang Jiang, and Margaret M. Redfield (Circ Heart Fail. 2012;5:720-726.); Olmsted County community cohort of HF patients (1984 to 2009).

Source: Cytokinetics, Incorporated