Cytokinetics Presents New Data in Patients With Non-Obstructive HCM From Cohort 4 of REDWOOD-HCM in Late-Breaking Clinical Trial Session at The European Society of Cardiology Heart Failure 2023 Congress
Treatment of Aficamten was Well-Tolerated and Associated with Statistically Significant Improvements in KCCQ, Angina Frequency, NYHA Class, NTpro-BNP and High-Sensitivity Troponin I
Phase 3 Clinical Trial in Non-Obstructive HCM To Begin in 2H 2023
SOUTH SAN FRANCISCO,
“We’re pleased to see that, in addition to the previously reported improvements in both functional class and cardiac biomarkers, patients with nHCM treated with aficamten in Cohort 4 of REDWOOD-HCM experienced a statistically significant improvement in patient reported health status, the KCCQ clinical summary score, an important measure of disease burden,” said
The new data from Cohort 4, presented today by
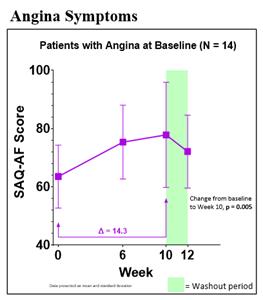
At 10 weeks, treatment with aficamten was associated with an average improvement in KCCQ-CSS of 10.6 points (p < 0.0001) (Figure 1). Overall, 58% of patients experienced a clinical reduction in symptom burden: 12.5% had a small improvement (≥ 5-10 points), 20% had a moderate to large improvement (≥ 10-20 points), and 25% had a large to very large improvement (≥ 20 points). Additionally, 56% of patients demonstrated improvement of ≥1
Figure 1: Kansas City Cardiomyopathy Questionnaire (KCCQ)
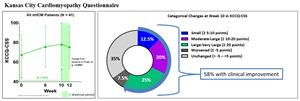
Figure 2: Angina Symptoms
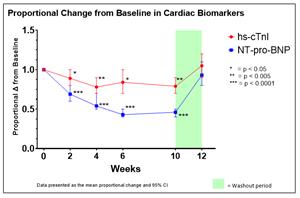
Figure 3:
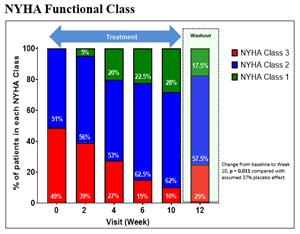
Treatment with aficamten was associated with a mean relative reduction in high-sensitivity cardiac troponin I of 21% by Week 10 with an absolute mean (SE) reduction of -24.8 ng/L (11.6; p < 0.005), and a mean relative reduction in NT-proBNP of 55% by Week 10 with an absolute mean (SE) reduction of -870 pg/mL (155.3; p < 0.0001) (Figure 4). After the 2-week washout period, NT-proBNP and high-sensitivity troponin I levels returned to baseline levels.
Figure 4: Cardiac Biomarkers
As previously reported, aficamten was generally well-tolerated. The most common adverse events reported were mild fatigue (9.8%) and dizziness (7.3%). By Week 6, 35 (85%) of patients achieved the highest available dose of 15 mg of aficamten, and 6 (15%) achieved 10 mg. From baseline to Week 10 there was a modest and reversible reduction in left ventricular ejection fraction (LVEF) of -5.5% (9.9%). There were no drug discontinuations due to adverse events, no treatment interruptions or down-titration events related to LVEF <50%, and no events with LVEF <40%. Three patients (7.3%) had LVEF <50% at Week 10; all three patients returned to baseline LVEF after the 2-week washout period, and none were associated with adverse events. No adverse events of heart failure were reported. Four patients (9.8%) had serious adverse events, including one previously reported death, and none were attributed to aficamten.
About REDWOOD-HCM
REDWOOD-HCM HCM (Randomized Evaluation of Dosing With CK-274 in Obstructive Outflow Disease in HCM) is a Phase 2, multi-center, randomized, placebo-controlled, double-blind, dose finding clinical trial of aficamten divided into 4 Cohorts. Cohorts 1, 2 and 3 enrolled patients with obstructive HCM (oHCM) and Cohort 4 enrolled patients with non-obstructive HCM (nHCM). In Cohorts 1 and 2, patients continued taking background medications exclusive of disopyramide. Results from Cohorts 1 and 2 showed that treatment with aficamten or 10 weeks resulted in statistically significant reductions from baseline compared to placebo in the average resting left ventricular outflow tract pressure gradient (LVOT-G) and the average post-Valsalva LVOT-G. 78.6% of patients treated with aficamten in Cohort 1 and 92.9% of patients treated with aficamten in Cohort 2 achieved the target goal of treatment, defined as resting gradient <30 mmHg and post-Valsalva gradient <50 mmHg at Week 10, compared to placebo. Patients treated with aficamten also saw improvements in heart failure symptoms and reductions in NT-proBNP, a biomarker of cardiac wall stress. Treatment with aficamten in REDWOOD-HCM was generally well tolerated and the incidence of adverse events on aficamten was similar to that of placebo. No serious adverse events were attributed to aficamten, and no treatment interruptions occurred on aficamten. Cohort 3 showed that aficamten was associated with reductions in LVOT-G and Valsalva LVOT-G, and improvements in NYHA Class and NT-proBNP in patients with obstructive HCM whose background therapy included disopyramide, with safety and tolerability consistent with Cohorts 1 and 2. Cohort 4 enrolled 41 patients with nHCM, who were
About Aficamten
Aficamten is an investigational selective, small molecule cardiac myosin inhibitor discovered following an extensive chemical optimization program that was conducted with careful attention to therapeutic index and pharmacokinetic properties and as may translate into next-in-class potential in clinical development. Aficamten was designed to reduce the number of active actin-myosin cross bridges during each cardiac cycle and consequently suppress the myocardial hypercontractility that is associated with hypertrophic cardiomyopathy (HCM). In preclinical models, aficamten reduced myocardial contractility by binding directly to cardiac myosin at a distinct and selective allosteric binding site, thereby preventing myosin from entering a force producing state. The development program for aficamten is assessing its potential as a treatment that improves exercise capacity and relieves symptoms in patients with HCM as well as its potential long-term effects on cardiac structure and function. Aficamten received Breakthrough Therapy Designation for the treatment of symptomatic obstructive HCM from the
About Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is a disease in which the heart muscle (myocardium) becomes abnormally thick (hypertrophied). The thickening of cardiac muscle leads to the inside of the left ventricle becoming smaller and stiffer, and thus the ventricle becomes less able to relax and fill with blood. This ultimately limits the heart’s pumping function, resulting in symptoms including chest pain, dizziness, shortness of breath, or fainting during physical activity. A subset of patients with HCM are at high risk of progressive disease which can lead to atrial fibrillation, stroke and death due to arrhythmias.
About
For additional information about
Forward-Looking Statements
This press release contains forward-looking statements for purposes of the Private Securities Litigation Reform Act of 1995 (the "Act").
CYTOKINETICS® and the
Contact:
Senior Vice President, Corporate Communications, Investor Relations
(415) 290-7757
Photos accompanying this announcement are available at
https://www.globenewswire.com/NewsRoom/AttachmentNg/6c258762-145b-4788-87af-90d32ffea42e
https://www.globenewswire.com/NewsRoom/AttachmentNg/4cbe99ba-8a16-46b3-b19b-f2270dddc3af
https://www.globenewswire.com/NewsRoom/AttachmentNg/572d9e3b-668c-4348-b801-8dfc1003d53a
https://www.globenewswire.com/NewsRoom/AttachmentNg/8ab8e516-4220-46e3-99d1-46f118819c62

Source: Cytokinetics, Incorporated